Abstract
PURPOSE
Asparaginase is a key component of acute lymphoblastic leukemia (ALL) therapy. Hypersensitivity reactions challenge its use and occur frequently (30-75%) after native Escherichia. Coli (E.coli) asparaginase (Appel et al., 2008; Muller et al., 2001; Panosyan et al., 2004; Silverman et al., 2001). The international ALL Ponte di Legno Toxicity Work Group (PTWG) classifies hypersensitivity to asparaginase as (i) allergy in case of symptoms of allergy (always associated with undetectable asparaginase activity levels), (ii) allergic-like reactions in case of symptoms without inactivation, and (iii) silent inactivation (SI) with inactivation of asparaginase activity, but without hypersensitivity symptoms (Schmiegelow et al., 2016). Allergic-like reactions and SI can only be diagnosed with monitoring of asparaginase activity levels. A meta-analysis was performed based on data from the PTWG to estimate the incidence of hypersensitivity and risk factors for hypersensitivity to asparaginase in ALL protocols using pegylated E.coli asparaginase (PEGasparaginase) as first line of treatment.
PATIENTS AND METHODS
Questionnaires were sent to all members of the PTWG. Information on protocol level regarding PEGasparaginase dose, dosing regimen (e.g. dosing frequency, total number of doses, PEGasparaginase-free intervals(s)), administration route, total induction and post-induction hypersensitivity rates per protocol and per risk group and use of therapeutic drug monitoring (TDM). To facilitate comparison between protocols with and without TDM, we defined allergic reactions as the sum of allergies and allergic-like reactions. Silent inactivation was analyzed separately.
RESULTS
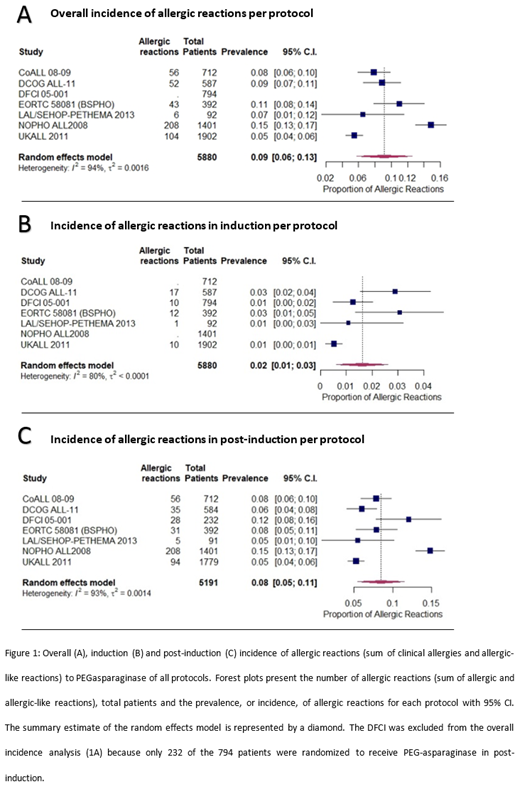
A total of 5880 patients with newly diagnosed ALL, aged 1 to 24 years old, were enrolled in seven different upfront ALL protocols using PEGasparaginase as first-line treatment. The overall incidence of allergic reactions along with 95% confidence interval (CI) were 9% [6%; 13%], 2% [1%; 3%] and 8% [5%; 11%] in the overall protocol, induction and post-induction, respectively (Figure 1). Severity of allergic reactions were described, according to the CTCAE version 3.0 or 4.03, per protocol. 47% of the reactions were classified as grade 3/4.
Univariate meta-regression analysis showed a positive association between the incidence of allergic reactions and number of PEGasparaginase-free intervals (P=0.005). High risk group stratification (P<0.001), post-induction treatment phase (P<0.001) and start of PEGasparaginase treatment in post-induction (P=0.006) were also associated with a higher incidence of allergic reactions. Route of administration (IV (8.9%, range 8.6-10.5%) versus IM (6.5%, range 5.5-14.8%)) did not significantly influence risk of hypersensitivity. Number of doses, duration of first PEGasparaginase-free interval and dosage did not significantly influence risk of hypersensitivity. Multivariate meta-regression analysis showed a positive association between the incidence of allergic reactions and the number of PEGasparaginase-free intervals (P=0.006) and start of PEGasparaginase in the post-induction treatment phase (P=0.02).
Two out of seven study groups reported an incidence of allergic reactions of 1.6-2.0%, which was 9-16% of all hypersensitivity. Three out of seven study groups reported an incidence of SI of 3.7-4.1%, which was 23-29% of all hypersensitivity reactions.
All protocols prescribed a switch to Erwinia asparaginase in case of clinical hypersensitivity and/or SI. 308 out of 348 (89%) of the patients with hypersensitivity to PEGasparaginase received Erwinia asparaginase. 19 out of these 308 (6%) exposed patients had an allergic reaction to Erwinia asparaginase, of which 7 out of 19 (37%) were grade 3/4.
CONCLUSION
The incidence of allergic reactions is lower in protocols using PEGasparaginase as first-line treatment compared to that reported for native E.coli asparaginase or PEGasparaginase after native E.coli asparaginase. Post-induction phase, a higher number of PEGasparaginase-free intervals, and initiation of PEGasparaginase in post-induction phase are risk factors for allergic reactions. These results are important for planning of PEGasparaginase administrations in future frontline therapy.
Albertsen: Erytech: Honoraria, Speakers Bureau; Servier: Speakers Bureau; BKA: Other: Sponsor of the investigator-initiated trial NOR-GRASPALL2016.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal